You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Obstructive sleep apnea (OSA) is a common form of chronic sleep-disordered breathing characterized by repetitive episodes of partial or complete upper airway obstruction, occurring in some patients as many as 100 times per hour.1,2 The resultant inadequate and fragmented sleep may lead to cognitive deficits, daytime somnolence, diabetes type 2, and cardiovascular morbidity and mortality such as strokes and heart attacks.1,3 For patients who visit the dentist frequently, the dental professional’s familiarity with the signs and symptoms of this disorder may prompt earlier referrals and greater predictability for further and successful treatment.
Two types of sleep apnea have been identified: central sleep apnea (CSA) and OSA.4 Of unknown etiology, CSA is suggested to be related to a variety of neurologic and intracranial lesions.1,5 CSA results from a mediated decrease or complete lack of respiratory drive evident by an absence of diaphragmatic and chest wall movement during sleep.1 The pathophysiology of OSA is markedly different and somewhat better understood. This type of sleep apnea is attributed to anatomical abnormalities resulting in partial occlusion or increased elasticity and compliance of the airway that allows for collapse during inspiration, thereby limiting airflow through narrow passages.1
Airway analysis has long been standard in orthodontic, OSA, and orthognathic evaluations. Historically, lateral cephalometric assays providing 2-dimensional (2D) analysis for diagnosis or predictions of post-treatment changes have been used. Lateral or frontal cephalometric measurements provide useful information for analyzing airway size in the mid-sagittal and single-layer coronal plane. However, with superimposition of 3-dimensional (3D) structures that does not adhere to strict right and left symmetry onto a 2D plane, a lack of identifiable soft-tissue contour in the third dimension leads to significant anatomic and volumetric measurement errors.6,7 This discrepancy between the viewed 2D configuration and the volumetric reality of the 3D structure results in inaccurate measurements and imprecise subsequent analyses. In addition, radiographically, the most physiologically relevant information is obtained in axial views, which are perpendicular to the direction of the airflow and are not visualized on the 2D images.8
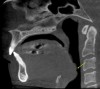
Computed tomography (CT) and cone-beam CT (CBCT) imaging technologies, unlike traditional 2D images in which superimposition of anatomic structures in the mid-sagittal plane obscures volumetric areas of interest, allow visualization and measurement of the airway in 2D planes as well as 3D volumetric analyses.4 Also unlike traditional 2D images, CBCT data is not magnified and is measured directly on (or close to) a 1:1 scale allowing greater clinical accuracy.1 Using various commercially available segmentation software programs, the clinician is able to study the planar and volumetric 3D images thoroughly (Figure 1).
Discussion
OSA is a potentially life-threatening condition characterized by repetitive full or partial upper airway collapse caused by mechanical or anatomic obstruction, resulting in diminution of airflow during sleep.1,2,9 With the patient in supine position, for example, gravitational forces displace the tongue and soft palate posteriorly, contracting the airway, causing obstruction and narrowing.3
In the United States, it is suggested that OSA affects approximately 20% of middle-aged patients who snore. According to Strauss et al, this equates to 4% of all middle-aged men and 2% of all middle-aged women.1,4,9,10 The actual incidence may, in reality, be higher; inaccurate diagnosis and lack of recognition or reporting may greatly lessen the number of known cases.1
In addition to surgical treatments, transient or permanent expansion of the retropalatal and retrolingual airway using nonsurgical approaches such as pedodontic and young adult appliance-enabled mandibular advancement, weight loss, behavior modifications (ie, changing sleep position, decreasing alcohol consumption), as well as continuous positive air pressure (CPAP) have been proposed as potential treatments.
Early Recognition
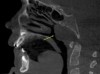
As more dentists become involved in the diagnosis and management of OSA, reliable diagnostic tools as well as better interpretive skills are in greater demand. Specifically, early diagnosis and treatment of pediatric sleep apnea may have a significant effect on quality of life. Compared to medical colleagues, dentists generally see pediatric or adult patients on a greater frequency and routinely examine the oropharynx where conditions such as tonsillar enlargement have been shown to be a prime cause of apnea (Figure 2).4 Early recognition and correct diagnosis offered by utilization of clinical findings and radiographic surveys common in dentistry provide important steps in evaluation of OSA.
The accuracy of CBCT in defining the shape and size of the airway has been confirmed by evaluation of calibrated acrylic airway models.8 CT provides 3D-reconstructed images from multiple planar projections.11 CBCT delivers similar images to CT with the advantage of rapid acquisition time, considerable lower radiation dose to the patient, and the ability to provide both multiple planes and 3D volumetric views from reconstruction of multiple sequential planar projections.11,12 CBCT/CT offers the ability to reorient images and/or adjust the histogram for better visualization.2 While CBCT provides some visualization of soft tissue by utilizing differentiation between gray-level intensities, the inability of CBCT units to provide strong soft-tissue contrast renders them inefficient in detailed soft-tissue pathology analysis.
Function of the upper airway may be divided into respiration, deglutition, and speech.2 Respiration requires patency of the upper airway, whereas deglutition and speech require selective narrowing or closure of the airway to prevent entry of external objects into the trachea or to aid phonation.2
Pharyngeal Airway
The upper respiratory tract is considered to include the structures above the trachea from the nostrils to the larynx. Patency of the pharynx, a section of the upper respiratory tract, as well as its ability to collapse is uniquely important.13 The pharyngeal airway is comprised of three gross sections:
The nasopharyngeal airway is the cone-shaped, upper-most section.11,13 It extends from the posterior nasal cavity to the level of the hard palate, with the posterior pharyngeal wall containing tonsillar tissues.3,13
The oropharyngeal airway extends from the posterior portion of the oral cavity, ranging inferiorly to the base of the tongue; it contains muscles, mucosa, adenoids, as well as a complex network of lymphatic tissues. The anterior boundary is composed of the soft palate, base of the tongue, and the anterior wall of the pharynx. A group of various muscles, adipose tissue, and the palatine tonsils form the lateral pharyngeal walls.3,11,13
The hypopharyngeal airway extends from the most superior tip of the epiglottis to the most inferior area of the airway at the larynx.13
Pathophysiology of OSA is thought to be related to narrowing or closure of the pharyngeal airway, resulting in respiratory effort to overcome the resistance pressure. McCrillis et al opined that the pharyngeal airway does not have a rigid support; instead it is formed and supported by muscles and ligaments.2 In patients who are imaged awake and in an upright position, the muscle tensions maintain patency. During sleep, the muscles relax, allowing the pharyngeal walls to become more flexible and collapsible. In supine position, gravitational effects, in addition to postural changes—for example, retropositioning of the tongue—necessitate higher velocity of air in order to exchange the desired volume of air through the narrowed airway lumen. The turbulent airflow results in fluttering and vibration of the flexible, narrowed pharyngeal walls and soft palate, thus producing snoring sounds.1
Anatomic Abnormalities
A variety of craniofacial anatomic abnormalities, including but not limited to enlarged tonsils and/or adenoids, hyperplasia of pharyngeal tissues, laryngomalacia (floppy epiglottis), long or enlarged soft palate, large or retropositioned tongue, skeletal abnormalities such as mandibular and maxillary hypoplasia, as well as normal structures with excessive movement and consequent prolapse into the airway during sleep, have been suggested in the etiology of OSA (Figure 3).1,9,13,14 For example, in comparison to similar age and sex controls, OSA patients who are still growing exhibit smaller retropalatal airway volume, with more concave, spherical, or elliptical upper airway morphology.15,16 More than half of apnea patients present with mandibular micrognathy and retrognathy in relation to the maxilla.1,6,9,16,17
In children and young adults, predisposing factors, repeated infections, or inflammation may increase the risk of adenotonsillar hypertrophy and the subsequent constriction of the posterior airway.13,15 Chronic conditions may be alleviated by mouth breathing.6
Role of Diagnostic Imaging
The role of diagnostic imaging is to evaluate the morphology and dimensions of the upper airway, including identification of the presence and location of any anatomic or pathologic obstruction. It is important to note that most radiographic evaluations are performed on static images.9 Those images commonly acquired with traditional 2D and CT/CBCT represent the patient in the moment of image acquisition only. In a passive state, without muscle activity, the cross-sectional dimensions of the airway are a function of the difference between the intraluminal and tissue pressure.17 Functional imaging studies use multiple scans acquired during different breathing phases to reveal the relationship between anatomy and physiology. In a functional state, airway size and shape are known to vary during the respiratory cycle.6 As such, the patient’s airway position, morphology, and dimensions may be influenced by his or her respiration and/or swallowing during image acquisition.4 Protocols such as placing the tongue in the roof of the mouth and abstaining from swallowing may minimize inspiratory and expiratory effects on static imaging. In interpreting the airway dimensions it should be emphasized that most of the views analyzed are static; they represent the moment in time when the scan was acquired and, without proper protocol, are subject to artificial findings.
The oropharyngeal airway located between the soft palate and the hyoid bone is an area of immense interest. Many authors have suggested a relationship between various malocclusion patterns and variations in the size and shape of this section of the airway.6 Patients identified as skeletal Class II often present with a forward inclination of the airway, whereas patients who are Class III present a more vertically oriented, larger, and flatter oropharyngeal region.1,15
Cephalometric and CBCT/CT studies are in agreement that at the level of the uvula and mandibular plane, OSA patients exhibit the narrowest sagittal and cross-sectional dimensions, respectively, with the greatest cross-sectional narrowing in patients with severe OSA.1,9
Factors such as increased body mass and/or obesity have been suggested to positively correlate with OSA. Due to the decrease in the lateral dimensions of the pharynx, the airway in patients with higher BMI tends to be more spherical, suggesting certain airway shapes may be greater predictors of airway collapse.1 Magnetic resonance studies, including those involving obese subjects, confirmed that greater fat surrounding the collapsible pharyngeal segment of OSA patients with increased neck soft tissue.1,9 With the exception of a few studies, the decreased volume of fat pads surrounding the lateral pharyngeal wall and parapharyngeal fat pads after weight loss is considered to significantly increase upper airway volume.1,9,18 Interestingly, OSA has also been diagnosed in some patients with normal weight and body mass index who presented with other predisposing factors.9
Cephalometric studies showed the length of the soft palate to be an average of 48 mm in individuals with OSA and 35 mm in healthy individuals.1 Studies have confirmed the presence of a longer and thicker soft palate in OSA patients, with a progressive increase in thickness as the severity of the disorder increases.9 Accuracy studies comparing manual and CBCT measuring methods have not shown significant differences.4
While relationship between narrowing of the oropharyngeal airway and presence of OSA is intuitive—and supported by findings in patients already diagnosed with the disorder—quantifying the dimensional limits of the airway to determine health versus disorder is more opaque. It is worth noting that human airway anatomy varies in size and morphology with different anteroposterior jaw positions affecting the total volume and anatomic areas of narrowing.15
Head posture and gravity during image acquisition will influence the morphology and volumetric representation of the upper airway.1,13,17 Most imaging techniques are done with the patient in an upright position and in an awake state; the major disadvantage is that the measurements do not reflect the patient’s natural sleeping position and, therefore, present the appearance of greater airway patency.1,9 Traditional supine CT/CBCT is useful in obtaining 3D airway data in positions that mimic sleep position. Upright units, which are used more commonly, provide general baseline assessment of the morphology and dimensions of the airway, allowing thorough evaluation of, for example, the pharyngeal recess, or the fossa of Rosenmüller, which is a prime location of nasopharyngeal carcinoma.15 In supine position, the effect of gravity may obscure the presence of hyperplastic cancerous tissues.
Conclusion
Patients who present with elevated risk of developing OSA include men, older individuals, and patients with high body mass index (≥ 29.9 kg/m2), craniofacial abnormalities, brachycephalic features, or hypertrophy or hyperplasia of soft tissues.10 Comparison of the upper airway between OSA-diagnosed and healthy patients is performed by measuring the minimum surface area, usually in the location(s) where narrowing is present, whether it is from the pharyngeal wall to the dorsum of the tongue or posterior to the soft palate.15
Radiographic findings alone are not pathognomonic for OSA; they should only serve to prompt the dental and medical team for further evaluation. The ability to examine cross-sectional and 3D imaging in addition to clinical and sleep study results will increase diagnostic and treatment planning accuracy. Precise anatomic analysis of the airway if correlated to the presence and severity of OSA will allow for greater predictability in diagnostic and treatment planning outcome. CBCTs do not provide soft-tissue contrast; as such, presence or absence of tissue fat pads cannot be appreciated. However, CBCTs are indispensable for many reasons, including: easy access to the units; lower radiation dose compared to traditional CT; nearly 1:1 image ratio in all three planes; the ability to easily manipulate the data in viewing planes of the clinician’s choice; the ability to easily measure; and the capacity to import standardized Digital Imaging and Communications in Medicine (DICOM) data sets into third-party OSA-specific software programs.4
Reproducible protocol during image acquisition prevents artificial narrowing of the airway. For example, in upright position scanners, an unnaturally posteriorly positioned head or tongue may create the perception of narrowing where it does not actually exist.17 To reach an accurate diagnosis a strict imaging protocol must be followed. In reaching a diagnosis, findings from clinical examination and lifestyle risk factors should be considered.17
CBCT imaging quality is related to scan time, radiation dose, patient positioning, and absence of patient movement during image acquisition. CBCT’s low-dose technique is a valuable tool. Understanding CBCT technology, including its limitations, will aid in proper interpretation. The use of CBCT for evaluating airway size and shape to confirm or rule out the presence of OSA, determining the severity of the existing condition, and predicting treatment outcomes offers considerable promise.4
DISCLOSURE
The author had no disclosures to report.
ABOUT THE AUTHOR
Mitra Sadrameli, DMD, MS
Private Practice, Chicago, Illinois, Clinical Assistant Professor, University of British Columbia, Vancouver, Canada; Diplomate, American Board of Oral Radiology;
REFERENCES
1. Yucel A, Unlu M, Haktanir A, et al. Evaluation of the upper airway cross-sectional area changes in different degrees of severity of obstructive sleep apnea syndrome: cephalometric and dynamic CT study. AJNR Am J Neuroradiol.2005;26(10):2624-2629.
2. McCrillis JM, Haskell J, Haskell BS, et al. Obstructive sleep apnea and the use of cone beam computed tomography in airway imaging: a review. Semin Orthod. 2009;15(1):63-69.
3. White SM, Huang CJ, Huang SC, et al. Evaluation of the upper airway morphology: the role of cone beam computed tomography. J Calif Dent Assoc. 2015;43(9):531-539.
4. Strauss RA, Wang N. Cone beam computed tomography and obstructive sleep apnea. Aust Dent J. 2012;57 suppl 1:61-71.
5. Kritzinger FE, Al-Saleh S, Narang I. Descriptive analysis of central sleep apnea in childhood at a single center. Pediatr Pulmonol. 2011;46(10):1023-1030.
6. Oh KM, Hong JS, Kim YJ, et al. Three-dimensional analysis of pharyngeal airway form in children with anteroposterior facial patterns. Angle Orthod. 2011;81(6):1075-1082.
7. Abramson ZR, Susarla S, Tagoni JR, Koban L. Three-dimensional computed tomographic analysis of airway anatomy. J Oral Maxillofac Surg. 2010;68(2):363-371.
8. Ghoneima A, Kula K. Accuracy and reliability of cone-beam tomography for airway volume analysis. Eur J Orthod. 2013;35(2):256-261.
9. El AS, El H, Palomo JM, Baur DA. A 3-dimensional airway analysis of an obstructive sleep apnea surgical correction with cone beam computed tomography. J Oral Maxillofac Surg. 2011;69(9):2424-2436.
10. Lenza MG, Lenza MM, Dalstra M, et al. An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res. 2010;13(2):96-105.
11. Kuo MC, Shih LY. Primary plasma cell leukemia with extensive dense osteosclerosis: complete remission following combination chemotherapy. Ann Hematol. 1995;71(3):147-151.
12. Dell'Aversana Orabona G, Salzano G, Iaconetta G, et al. Facial osteomas: fourteen cases and a review of literature. Eur Rev Med Pharmocol Sci. 2015;19(10):1796-1802.
13. Guijarro-Martinez R, Swennen GR. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;40(11):1227-1237.
14. Lohse AK, Scarfe WC, Shaib F, Farman AG. Obstructive sleep apnea-hypopnea syndrome: clinical applications of cone beam CT. Australasian Dental Practice. 2009;Sep/Oct:104-114.
15. Schwab RJ. Upper airway imaging. Clin Chest Med. 1998;19(1):33-54.
16. Rintala A, Nordström R, Partinen M, et al. Cepalometric analysis of the obstructive sleep apnea syndrome. Proc Finn Dent Soc. 1991;87(1):177-182.
17. Rivlin J, Hoffstein V, Kalbfleisch J, et al. Upper airway morphology in patients with idiopathic obstructive sleep apnea. Am Rev Respir Dis. 1984;129(3):355-360.
18. Akan H, Aksöz T, Belet U, Sesen T. Dynamic upper airway soft-tissue and caliper changes in healthy subjects and snoring patients. AJNR Am J Neuroradiol. 2004;25(10):1846-1850.