You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
One of the most important objectives for an interdisciplinary team should be optimization of the definitive restorative procedures to maximize long-term function, esthetics, and stability.1,2 Frequently, this requires orthodontic therapy to address optimally the underlying dentofacial problems. Orthodontists, like other members of the team, are searching continually for science-based treatment options to better address the needs and concerns of patients and to achieve better treatment acceptance. This need is true especially for adult patients whose problems can prove much more difficult to treat than children’s because of the inherent lack of growth. To further complicate the problem, orthognathic surgical options are being selected less often even though they are the optimal choice for the treatment of skeletal discrepancies. At the same time, patients of all age groups are demanding shorter treatment times.
These are just some of the reasons for alternative techniques for the development of surgically facilitated orthodontic therapy (SFOT). SFOT techniques, using corticotomies and single- or multiple-tooth osteotomies to enhance orthodontic movements, are gaining more popularity. When providers first hear about these techniques and the shortened treatment times, their initial reaction tends to be that of skepticism. Most doubt whether they could justify referring their patients for surgery simply to hasten orthodontic tooth movement. However, on closer evaluation, these techniques provide some very promising concepts to enable better overall treatment for patients with complex problems. Although these procedures are scientifically based, more clinical evidence and better protocols are needed before they gain wide acceptance as viable treatment options.
Several different types of SFOT are gaining momentum worldwide, and providers will certainly learn more about them in the future. All members of the interdisciplinary team should remain open-minded regarding the potential for these procedures, yet continue to be critical as to their scientific justification. This article provides a brief history and overview of SFOT, discusses the current diagnostic and treatment protocols, and illustrates clinical examples.
Background
The surgical procedures utilized in SFOT were described in dental literature as early as 1892.3 One of the more important articles was written in 1959 when Heinrich Kole suggested the greatest resistance to tooth movement is created by the cortical bone of the alveolus.4 He described the use of interdental corticotomies to facilitate accelerated orthodontic tooth repositioning three-dimensionally. Soon after Kole’s article, many authors described orthognathic-surgical techniques for correcting overall maxillary and mandibular skeletal discrepancies.5-7 Kole’s corticotomy procedures never became popular, probably because of the limited orthodontic appliances and techniques available to support them, as well as advancements in orthognathic surgery. Today, however, for numerous reasons, including the recent decline in the number of orthognathic surgeries, there is a tremendous renewed interest in alternative surgical options that can augment orthodontic and interdisciplinary outcomes.
The most widely known benefit of the modern SFOT procedures is faster tooth movement; some claim three to four times quicker than traditional orthodontic tooth movement.8 Shorter treatment time might be motivation for the patient; however, the interdisciplinary team should consider these techniques as a means for expanding the traditional boundaries of orthodontic therapy and providing viable solutions to problems that previously were very difficult, at best, to correct. More importantly, these procedures can modify the dentoalveolar complex so that the teeth, alveolar bone, and skeletal components can be appropriately addressed for maximizing ideal functional and esthetic relationships. In addition, these techniques also could reduce root resorption9 and provide a more stable result than traditional cell-mediated tooth movement alone.10 SFOT provides a viable option for addressing adult alveolar bone volume deficiency problems to create broader, more robust dental arches similar to what has been observed in ancient skeletons from prior to our modern refined diet. (Please see Origins of Dental Crowding and Malocclusions: An Anthropologic Perspective in the June 2009 Compendium.) In addition to correcting numerous interdisciplinary dental-facial problems, these arches also are perceived as more esthetically appealing in modern society.11
Diagnosis and Treatment Planning
For the team to better understand how these procedures can help, it is most helpful if each member diagnoses and plans the treatment in terms of the underlying problem(s) causing the dental malocclusion. The Fundamental Components of Dentofacial Problems12 (Figure 1) is a simplified classification system that the team can use to address these underlying problems. This process also helps ensure that the correct components are being treated to maximize the long-term results and minimize compromises.
Addressing all the fundamental components is important when optimally treating a malocclusion (especially the dental component, eg, worn, broken, or misshapen teeth). However, this article focuses on those involving alveolar bone, specifically the dentoalveolar and alveoloskeletal components. Malocclusion problems involving skeletal component discrepancies are best managed with traditional orthognathic surgery, or in extreme deformities, with distraction osteogenesis. These procedures that specifically address the overall skeletal issues might be more appropriately classified as orthodontically facilitated surgical therapies (OFST).
Dentoalveolar is defined as “of, relating to, or involving the teeth and their sockets.”13 In the fundamental components (Figure 1), this definition is interpreted as including the relationship of the teeth to the alveolar bone and to each other. This meaning also includes the quality and volume of alveolar bone housing the teeth, dental implants, or potential implant sites. Various dentoalveolar surgeries, such as extractions, bone grafting, and even implant therapy to replace missing roots, are used to treat some of the problems in this category. Optimal treatment for most tooth-to-bone and tooth-to-tooth relationship issues ideally involves some type of orthodontic therapy.
The alveoloskeletal fundamental component involves the relationship of the dentoalveolar complex to its skeletal base. Alveoloskeletal is not a frequently used term, but the authors find it very useful in describing malocclusions and esthetic problems related to a dentoalveolar complex that does not align properly with its associated skeletal base (eg, severe dentoalveolar retrusion or transverse deficiency of the maxillary arch). Orthodontics and dentofacial orthopedics performed at the ideal time in a patient’s growth and development can be effective in addressing these issues.14 However, options for specifically treating alveoloskeletal problems in adults have been very limited until now.
To better explain the importance of these alveolar bone components in treating malocclusions, it is helpful to review the overall goals and limitations of orthodontic therapy.14-16 Orthodontic goals for an interdisciplinary case should be to maximize tooth movement as needed to properly correct or compensate for the underlying discrepancies, while simultaneously minimizing iatrogenic tissue loss (such as root resorption, gingival recession, and bone loss) and finishing with a stable result. Traditional cell-mediated orthodontic tooth movement is an excellent option to accomplish these goals in most of the mild-to-moderate malocclusion problems, but it has limitations in more complex cases. The confines that can lead to iatrogenic tissue loss typically involve the cortical plate, especially buccal and lingual to the apices of the teeth. This is the area that has been referred to in the literature as the “orthodontic walls”15,17 (Figure 1). The level of their importance depends on which fundamental components are the actual underlying problems of the malocclusion.
For instance, in true skeletal discrepancies, the orthodontic limitations can become critical to the extent that addressing the underlying skeletal problem with orthognathic surgical procedures may be the only option to predictably treat to a favorable outcome. Many complex cases exist in which the underlying discrepancies are not skeletal problems but instead are alveolar bone discrepancies. Alveolar bone discrepancies could result from either a dentoalveolar problem, such as an alveolar bone deficiency that fails to allow enough room for the dentition, or an alveoloskeletal problem in which the dentoalveolar complex does not align properly with its associated skeletal base. Unlike skeletal discrepancies, alveolar bone discrepancies in adult patients represent underlying problems that historically clinicians had no ideal way to treat without compromise.
Orthodontists know from experience that cases with severe alveolar bone deficiencies can be difficult, at best, to treat with cell-mediated orthodontic tooth movement alone. In adults, this treatment approach traditionally requires long treatment times in which the orthodontist might have to compromise relationships, esthetics, and stability through either tooth extraction or by positioning the teeth outside the confines of their underlying bone. Compromising the case through extraction can lead to straighter teeth in a stable relationship, but the result might negatively affect dentofacial esthetics related to the position of the teeth to the face and possibly reduced lip support. Improved esthetics sometimes can be attained in these cases with nonextraction orthodontic therapy, but final tooth positions may violate the confines of the underlying bone and result in unstable relationships with a greater potential for iatrogenic tissue loss. Even more difficult to treat are severe alveoloskeletal discrepancies in which the dentoalveolar complex does not align properly with its associated skeletal base. Historically, there has not been a good viable option to treat this underlying problem without either overtreating the skeletal component with orthognathic surgery or violating the orthodontic walls through orthodontics alone. Alveolar bone volume deficiencies and alveoloskeletal or borderline skeletal discrepancies are excellent indications for SFOT.18 Figure 1 (bottom) displays the authors’ clinical interpretation of the effectiveness of the various treatment options in treating malocclusions involving dentoalveolar, alveoloskeletal, or skeletal fundamental components.
Surgical Techniques
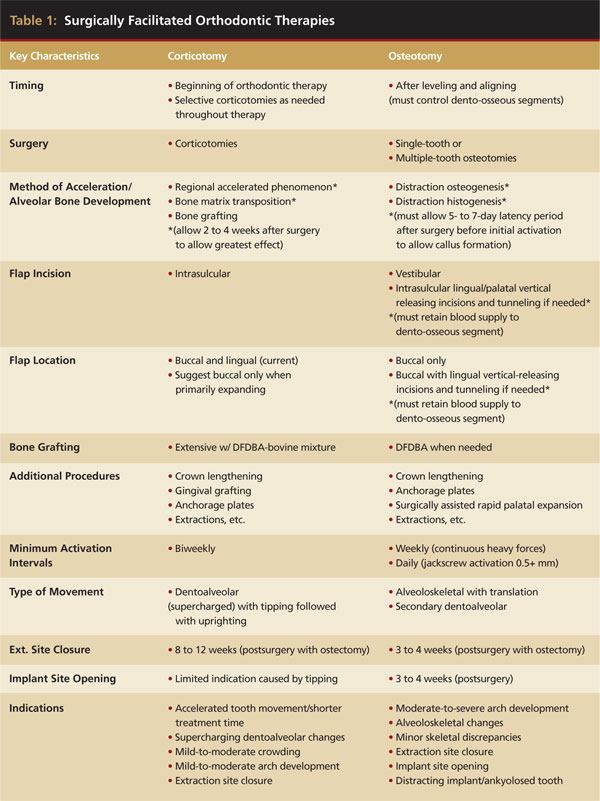
For describing the overall philosophies for the surgical techniques, the various facilitation procedures are divided into two categories: 1) those primarily using corticotomies or decortication and 2) those utilizing single- or multiple-tooth osteotomies. A corticotomy is a surgical technique in which only the cortical bone is cut, perforated, or mechanically altered to the depth of the medullary bone and the medullary bone remains intact. In contrast, an osteotomy consists of surgical cuts through both the cortical and medullary bone and typically indicates the creation of a bone segment. Table 1 differentiates between these two categories and outlines their various protocols.
Corticotomy Facilitated
The techniques in the corticotomy-facilitated category revolve around various methods of partially decorticating the alveolar bone housing the teeth to be moved (Figure 2 through Figure 10). Some of the techniques suggest buccal and lingual corticotomies19 while others recommend corticotomies just on the buccal to promote expansion. Some techniques routinely recommend extensive bone grafting in an attempt to facilitate bone development, while others do not. All of the corticotomy techniques primarily focus on weakening the cortical bone-tooth interface. Frost, an orthopedic surgeon, in his description of bone repair, suggested one of the desired effects of decortication.20 Physiologically, this theory proposes that when bone is injured or decorticated, it initiates a normal healing process with exuberant bone remodeling that is directly related to degree and proximity of the bone trauma. Frost named this process regional acceleratory phenomenon (RAP).20 Since then, this theory has been rigorously studied and proposed as a method of accelerating orthodontic treatment by other researchers.19,21-23 Numerous animal studies have shown up to a five-fold increase in medullary bone turnover in areas adjacent to corticotomy sites.24 It is speculated that this high medullary bone turnover in healthy tissues results in new bone formation and low bone density, which are conditions that promote rapid tooth movement with less root resorption.25 In addition, Chung et al and others claim that corticotomies combined with heavy forces lead to histologic changes called compression osteogenesis, in which the medullary bone of the decorticated segment can be bent to expand the traditional boundaries of orthodontic treatment.26
In the authors’ experience, corticotomies appear to “supercharge” traditional orthodontic therapy and make the associated dentoalveolar complex more plastic and malleable. This is very effective in accelerating orthodontic rotation and tipping movements and in helping moderate-arch development (Figure 11 through Figure 13). After healing, results appear to be very stable,10 probably because of reduced tissue memory as compared with traditional orthodontic tooth movement.18 To reduce the number of surgeries, periodontal grafting and crown-lengthening procedures can be combined with the corticotomies (Table 1).
 |
Osteotomy Facilitated
The second category of SFOT involves single- or multiple-tooth osteotomies and the physiologic principles of “distraction osteogenesis”23,27-32 (Figure 14 through Figure 33). Distraction osteogenesis is well described in the literature as a technique that allows changes in the vectors of growth and results in the genesis of new tissues.33,34 This biologic process begins when traction is applied to separate osteotomized bony segments and continues as long as the tissues of the callus that forms between the segments are stretched (Figure 33). This stretching across the surgical site also initiates distraction histogenesis of the soft tissues surrounding the distracted bone, leading to proliferation of ligaments, muscle, blood vessels, gingiva, and nerve tissue.
The osteotomy-facilitation technique that the authors have been using for many years is called dentoalveolar distraction osteogenesis (DDO).18 Orthodontic appliances serve as tooth-borne distracters instead of the bone-borne distracters used in traditional distraction osteogenesis. The orthodontist must use much more aggressive movement with osteotomies compared with corticotomies to maximize the distraction principals. With DDO, vertical osteotomies are placed between the teeth into the interradicular bone. To preserve the vitality of the teeth, only horizontal corticotomies are completed through the cortex just apical to the root apices (Figure 33). The individual dento-osseous segments then are gently luxated to create a greenstick fracture.35 If the osteomized segments are to be rotated or torqued, the bony cuts are needed to allow movement three-dimensionally. Extra decortication may be necessary because any cortical-bone-to-cortical-bone contact of the segments will stop movement and prevent further distraction osteogenesis. Demineralized freeze-dried bone is grafted in the osteotomy sites and other areas when augmentation is needed. Platelet-rich plasma also can be used to enhance soft-tissue healing. After a latency, or initial healing period of 5 to 7 days, the orthodontist can use the associated tooth as a handle to bodily move the osteotomized alveolar segment in relationship to its skeletal foundation by applying heavy orthodontic or orthopedic mechanics. The RAP effect from the surgery might further enhance and accelerate cell-mediated tooth movement.
DDO, in conjunction with either closing extraction sites or opening implant sites, has been an ideal tool for treatment of severe anterior-posterior alveoloskeletal discrepancies that otherwise might have been overtreated with orthognathic surgical procedures even though the underlying skeletal foundation is in a relatively normal position (Figure 14 through Figure 33). DDO even has been used to reposition implants36 and ankylosed teeth37 to more ideal positions (Table 1). After healing, the alveolar changes associated with DDO have remained stable, probably because of the effects of distraction osteogenesis and distraction histogenesis.
The SFOT corticotomy and osteotomy procedures are performed on an outpatient basis and have significantly less cost, recovery time, and morbidity as compared with traditional orthognathic surgical procedures.
Timing and Orthodontic Considerations
When using SFOT, orthodontists will have to modify some of their traditional approaches depending on the type of alveolar problem. If the discrepancies are primarily dentoalveolar (such as severe crowding with alveolar bone deficiency), corticotomy surgery typically is performed within 2 weeks of orthodontic appliances placement (Figure 4 and Figure 10). This early surgery appears to maximize the alveolar correction and minimize the negative compromises from cell-mediated tooth movement alone in a deficient alveolus.
When the underlying problem is an alveoloskeletal discrepancy (such as severe dentoalveolar retrusion or protrusion), the osteotomy surgery should be performed after orthodontic leveling and aligning has been completed (Figure 33). This allows the orthodontist to use rigid arch wires during and after surgery to better control the osteotomized dentoalveolar segments. This control is needed especially when combining osteotomies with absolute anchorage (dental implants, mini-implants, and plates) (Figure 18) and with orthopedic forces utilizing a jackscrew-type appliance38 (Figure 25 through Figure 28) to further modify the alveoloskeletal relationships. Selective corticotomies occasionally are performed in the middle stages of orthodontic therapy to facilitate individual tooth movement or to aid in dentoalveolar intrusion with anchorage plates after control has been established using rigid arch wires.
When combination problems involve dentoalveolar and alveoloskeletal discrepancies, the team needs to choose a type of surgery and decide if multiple-stage surgeries are needed to best address the problems individually. Selective corticotomies are performed frequently at the osteotomy surgery to deal with moderate combination problems (Figure 18). In more severe cases, corticotomies could be performed at the beginning of orthodontic therapy to enhance and accelerate dentoalveolar correction, and then a second surgery with osteotomies could be executed for alveoloskeletal correction after control has been established.
Generally, the orthodontic activation for most surgical-facilitation procedures begins after a 5- to 7-day latency period in accordance with distraction principles. Published distraction regimens of 0.5 mm/day are used to safely move osteotomized bone segments with minimal risk of devitalization. The patient is seen as often as needed until the desired alveolar correction is achieved with minimal appointment intervals being weekly for osteotomy facilitation and biweekly for corticotomy facilitation. Distraction osteogenesis procedures require continuous heavy forces (with heavy springs or elastics) or, more ideally, controlled daily activation with a jackscrew appliance by either the orthodontist or patient. During the postsurgical orthodontic phase, it is important to maintain active forces to maximize the effects of the surgical facilitation. This not only increases the speed of changes, but also helps prevent complete healing of the surgical sites and thereby prolongs the acceleration and distraction effects.
Case Reports
Four case reports illustrate various principles of SFOT. Case 1 (Figure 2 through Figure 9) involves a patient with some complex anterior restorative needs that required dentoalveolar correction. Maintaining esthetics during treatment and minimizing the length of time of orthodontic therapy were primary concerns. This was a perfect indication for corticotomy. The dentition was restored optimally to a stable result after only 5 months of restorative-driven orthodontics. Case 2 (Figure 11 through Figure 13) also used corticotomy but illustrates some of its limitations. The technique facilitated reopening of first premolar extraction sites to enable optimal restoration on the worn dentition and correction of the insufficient lip support. The patient ideally needed alveoloskeletal correction, and the corticotomies facilitated only dentoalveolar correction with excessive tipping. Osteotomy would have been a better choice.
Cases 3 and 4 illustrate using osteotomy for alveoloskeletal correction of some complex foundation issues. Case 3 (Figure 14 through Figure 23) is an excellent example of using interdental osteotomies, traditional orthodontic appliances, anchorage plates, and the principles of distraction osteogenesis to develop new alveolar bone and significantly change the relationship of dentoalveolar complex with its skeletal base. Buccal corticotomies also were used for lateral expansion. Ideal implant sites were created, and dentofacial esthetics were enhanced tremendously. Case 4 (Figure 24 through Figure 32) combines single- and multiple-tooth osteotomies with orthopedic forces applied through jackscrews to maximize control and distraction osteogenesis. This approach appears to be the trend for osteotomy and ideal for opening implant sites or closing extraction spaces. As this case illustrates, it also is optimally suited for alveoloskeletal correction, especially when combined with skeletal anchorage. No other approach, including orthognathic surgery, would have established the foundation as ideally for restorative therapy.
Contraindications and Potential Complications
Contraindications to SFOT include active periodontal disease, insufficient attached gingiva, dental caries, uncontrolled diabetes mellitus, compromised immune systems, and patient incompliance. SFOT is not recommended for patients taking medications that alter bone metabolism, such as bisphosphonates and long-term corticosteroids. Non-steroidal anti-inflammatory drugs may counteract some of the effects of these procedures and should be avoided.
After treating more than 100 surgically facilitated cases, the authors have encountered surprisingly few complications. Most involved some type of gingival recession, including some minor black triangles that were closed after reshaping of the interproximal contacts. The most significant problems, understandably, occurred with the more aggressive osteotomy procedures. These included severe gingival recession because of improper flap design, four devitalized teeth (required root canals), and five teeth that ankylosed before final orthodontic positioning. The devitalization and ankylosis problems occurred in cases in which the osteotomies were performed early in orthodontic therapy (before leveling and aligning), and the osteotomized segments were moved significantly during surgery without undergoing a latency period. Some issues arose because traditional orthodontic appliances were used for tooth-borne distraction osteogenesis and these simply did not have enough strength. New appliances need to be designed that are easier to work with and will provide adequate control while applying the needed forces.
These surgical and orthodontic procedures are clearly technique-sensitive and entail much more than can be covered in a brief review such as this. More information on SFOT is appearing in the literature, and textbooks and seminars are being dedicated entirely to this topic.39 It is strongly recommended that the entire interdisciplinary team study these techniques in detail before attempting them.
Conclusion
In this review, exciting new concepts were presented that address dentoalveolar and alveoloskeletal discrepancies using corticotomies, interdental osteotomies, dentoalveoalar distraction osteogenesis, and active orthodontics. These techniques have significantly changed the way many providers diagnose and treat. SFOT procedures are likely to gain greater acceptance as more clinical evidence emerges and more refined protocols become available.
References
1.Roblee RD. A comprehensive approach to dentofacial treatment. In: Bell WH, ed. Modern Practice in Orthognathic and Reconstructive Surgery. Philadelphia, PA: WB Saunders Co. 1992:1736.
2.Roblee RD. Interdisciplinary Dentofacial Therapy: A Comprehensive Approach to Optimal Patient Care. Hanover Park, IL: Quintessence Inc.; 1994.
3.Wescott A. A case of irregularity. Dental Cosmos. 1859;1:60-68.
4.Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959;12(5):515-529.
5.Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957;10(7):677-689.
6.Bell WH. Lefort I osteotomy for correction of maxillary deformities. J Oral Surg. 1975;33(6):412.
7.Bell WH, Epker BN. Surgical-orthodontic expansion of the maxilla. Am J Orthod. 1976;70(5):517-528.
8.Hajji SS, Ferguson DJ, Miley DD, et al. The influence of accelerated osteogenic response on mandibular decrowding. J Dent Res. 2001;80:180.
9.Iino S, Sakoda S, Ito G, et al. Acceleration of orthodontic tooth movement by alveolar corticotomy in the dog. Am J Orthod Dentofacial Orthop. 2007;131(4):448.
10.Nazarov AD, Ferguson DJ, Wilcko WM, et al. Improved retention following corticotomy using ABO Objective Grading System. J Dent Res. 2004;83:2644.
11.Sarver DM, Ackerman MB. Dynamic smile visualization and quantification: Part 2. Smile analysis and treatment strategies. Am J Orthod Dentofacial Orthop. 2003;124(2):116-127.
12.Roblee RD. Paper presented at: Interdisciplinary Care Conference: Five Disciplines, One Focus. February 2001; Dallas, TX: American Association of Orthodontists.
13.Dentoalveolar. Merriam-Webster Medical Dictionary. http://merriam-webster.com/medical/dentoalveolar. Accessed November 20, 2018.
14.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics. 4th ed. St. Louis, MO: Mosby; 2006.
15.Handelman CS. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66(2):95-109.
16.Melsen B. Limitations in adult orthodontics. In: Melsen B, ed. Current Controversies in Orthodontics. Hanover Park, IL: Quintessence; 1991:147-180.
17.Edwards JG. A study of the anterior portion of the palate as it relates to orthodontic therapy. Am J Orthod. 1976;69(3):249-273.
18.Bolding SL, Roblee RD. Optimizing orthodontic therapy with dentoalveolar distraction osteogenesis. In: Bell WH, Guerrero CA, eds. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Ontario: BC Decker; 2007:167-186.
19.Wilcko MW, Wilcko T, Bouquot JE, et al. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21(1):9-19.
20.Frost HM. The regional accelerated phenomenon. Orthop Clin N Am. 1981;12:725-726.
21.Wilcko MT, Wilcko MW, Marquez MG, et al. The contribution of periodontics to orthodontic therapy. In: Dibart S, ed. Practical Advanced Periodontal Surgery. Hoboken, NJ: Wiley-Blackwell; 2007:23-50.
22.Wilcko TM, Wilcko WM, Omniewski KB, et al. The periodontally accelerated osteogenic orthodontics (PAOO) technique: efficient space closing with either orthopedic or orthodontic forces. Journal of Implant and Advanced Clinical Dentistry. 2009;1(1):45-63.
23.Lee W, Karapetyan G, Moats R, et al. Corticotomy-/Osteotomy-assisted tooth movement microCTs differ. J Dent Res. 2008;87(9):861.
24.Bogoch E, Gschwend N, Rahn B, et al. Healing of cancellous bone osteotomy in rabbits–Part I: regulation of bone volume and the regional acceleratory phenomenon in normal bone. J Orthop Res. 1993;11(2):285-291.
25.Twaddle BA, Ferguson DJ, Wilcko WM, et al. Dento-alveolar bone density changes following accelerated orthodontics. J Dent Res. 2002;80:301.
26.Chung K, Kim S, Kook Y. Speedy surgical orthodontic treatment with skeletal anchorage in adults. In: Bell WH, Guerrero CA, eds. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Canada: B.C. Decker, Inc.; 2007.
27.Snyder CC, Levine GA, Swanson HM. Mandibular lengthening by gradual distraction. Preliminary report. Plast Reconstr Surg. 1973;51(5):506-508.
28.Wagner H. Surgical lengthening or shortening of femur and tibia. In: Hungerford DS, ed. Progress in Orthopedic Surgery. Berlin, Germany: Springer-Verlag; 1977.
29.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;(239):263-285.
30.Van Sickels JE. Need for distraction osteogenesis. In: Bell WH, Guerrero CA, eds. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Canada: B.C. Decker, Inc.; 2007.
31.Chin M, Toth BA. Distraction osteogenesis in maxillofacial surgery using internal devices: review of five cases. J Oral Maxillofac Surg. 1996;54(1):45-53.
32.Guerrero CA, Lopez P, Figueroa F, et al. Three-dimensional alveolar distraction osteogenesis. In: Bell WH, Guerrero CA, eds. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Canada: B.C. Decker, Inc.; 2007.
33.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;(239):263-285.
34.Cope JB, Samchukov ML, Cherkashin AM. Mandibular distraction osteogenesis: a historic perspective and future directions. Am J Orthod Dentofacial Orthop. 1999;115(4):448-460.
35.Bell WH. Immediate surgical repositioning of one- and two-tooth dento-osseous segments. Int J Oral Surg. 1973;2(6):265-272.
36.Gotta S, Sarnachiaro GO, Tarnow DP. Distraction osteogenesis and orthodontic therapy in the treatment of malpositioned osseointegrated implants: a case report. Pract Proced Aesthet Dent. 2008;20(7):401-405.
37.Kofod T, Würtz V, Melsen B. Treatment of an ankylosed central incisor by single tooth dento-osseous osteotomy and a simple distraction device. Am J Orthod Dentofacial Orthop. 2005;127(1):72-80.
38.Sukurica Y, Karaman A, Gürel HG, et al. Rapid canine distalization through segmental alveolar distraction osteogenesis. Angle Orthod. 2007;77(2):226-236.
39.Bell WH, Guerrero CA, eds. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Canada: B.C. Decker, Inc.; 2007.
About the Authors
Richard D. Roblee, DDS, MS, Adjunct Associate Professor, Department of Orthodontics and Department of Restorative Sciences, Baylor College of Dentistry, Dallas, Texas; Private Practice, Fayetteville, Arkansas
Scotty L. Bolding, DDS, MS, Private Practice, Fayetteville, Arkansas
Jason M. Landers, DDS, MS, Private Practice, Fayetteville, Arkansas