You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Dr. J. Wesley Alexander reported that uses of silver date back centuries BC,1asPersian kings drank water that was transported only in silver vessels. They had no knowledge of microbes, but did know that the water remained fresh. Silver preparations were later used by Hippocrates (460-377 BC) to promote wound healing and treat ulcers. Alexander also noted that silver nitrate was most probably used as a medical preparation "because it was mentioned in a pharmacopeia published in Rome in 69 BCE."1
The use of silver solutions to treat dental caries has been advocated since the mid-1800s. In 1916, Prinz wrote, "As early as 1846 we read in the ‘Zahnarzt' (a German dental publication) that the application of silver nitrate to carious surfaces on teeth is very beneficial, as it ‘practically stops the progress of the carious process.'… A number of prominent practitioners-Clark, Chupein, Shanasy, Tomes, Salter, Bauer, Black, Miller, Pierce, Conrad, and many others-have greatly lauded the value of silver nitrate as a means of abating the progress of dental caries, and especially Taft (Taft: Operative Dentistry, 1859, p. 214.), as early as 1859, expresses himself most favorably on this subject."2Pedley's 1895 book refers to silver nitrate six times as treatment for tooth sensitivity and caries attentuation.3 In 1924, Hogeboom4 and Black,5 in their respective textbooks, explained the use of silver nitrate for treatment of caries lesions, including illustrations of how the solution turns caries lesions black.
In North America, a dramatic resurgence of interest in using silver to affect dental caries infection dynamics occurred in 2015 with the market introduction of a 38% silver diammine fluoride solution (Advantage Arrest™, Elevate Oral Care, elevateoralcare.com).6,7
The product was granted 510(k) premarket notification (approval) as substantially equivalent to fluoride varnish in desensitizing teeth. The blue-tinted silver diammine fluoride formula is Ag(NH3)2F, with a component breakdown of6:
• Silver (Ag) 24-27%
• Ammonia (NH3) 7.5-11%
• Fluoride (F) 5-6%
• FD&C Blue #1 < 1%
• Deionized Water <=62.5%
Note: "diammine" is commonly and erroneously known as "diamine."8,9 In this report, the product will be referred to as "silver diammine fluoride" or "SDF."
Scientific and commercial dentistry journals since 2015 have been replete with writings about clinical techniques, individual and academic institution protocols, case documentations, and research reports about off-label use of the product as a caries "arresting" agent.10-17 For example, the Journal of the California Dental Association devoted the January and February 2018 issues solely to articles about silver diammine fluoride.
SDF should more accurately be referred to as a caries infection delaying or intercepting agent, rather than a solution that "arrests" caries progression, which connotes stopping or cessation of microbial activity. Perhaps Prinz, in 1916, said it best when he used the word "abating," referring to silver nitrate's action on dental caries lesions, which now can be similarly attributed to SDF.2 Studies show that silver diammine fluoride does affect dental caries lesions, but bacteria survives in varying levels within those lesions.18,19However, any discussion of the influence of SDF on caries lesions must take into account the cumulative effect of multiple applications over varying time intervals, which can be part of a treatment plan. Microbiologists (and verbivores) might suggest that "attenuation" of the caries infection by the silver solutions is a particularly apt term.
Treatment Considerations
There are many factors in the decision to use SDF in children's dentistry, as examined in a recent roundtable discussion on the subject.20 These include:
• Parents' feelings about their children's treatment plans. Perhaps the most important consideration is the parents' or caretakers' attitude about SDF treatment, once they are educated about the implications of SDF and alternative treatment plans. As parental consent is required, the dentist needs to explain the options so that parents are comfortable with their decisions for their children.
• Patient's ability to tolerate and cooperate for chairside dental treatment without having to resort to pharmaceutical behavior management, besides the routine use of nitrous oxide/oxygen inhalation.
• Age of patient. SDF application on Class II caries lesions of primary molars in a 10-year-old might be an ideal plan for teeth that will exfoliate within a year or two, but traditional restorative care in a younger child might preclude additional clinical intervention, and be a better choice in the long run.
• Anatomical location and extent of caries lesion. Parents are usually more willing to consent to black-stained lesions in posterior teeth than in teeth that show.
• Patient safety. If easy application of SDF can delay or eventually preclude the need for sedation or general anesthesia, perhaps the patient can be treated with routine restorative care later. Avoiding or delaying the need for local anesthetic injections and postoperative tissue numbness in very young children are additional advantages.
• Finances and speed of treatment. Application of SDF takes a fraction of the time it would take for routine dental restorative procedures and thus should be much less expensive for families.
• Pain relief. In children whose carious teeth are sensitive, SDF can serve an agent of immediate interim relief while comprehensive treatment planning is completed.
Applications
The patients pictured in this report represent a wide scope of silver diammine fluoride treatment for children. These patients were treated in a similar manner to the general protocol recommended by TRAC Research, with some modification19:
blot dry the surface of the caries lesion (cotton swab, air syringe)
paint on the silver diammine fluoride and continue to dab it (avoid oversaturating to prevent overflow to soft tissues)
keep lesion isolated for 60 seconds, blot with cotton swab to soak up excess, and then cover the region with fluoride varnish
repeat same treatment several months later, then reapply at 6-12 month intervals.
Silver diammine fluoride solution needs to be handled carefully. Staining of skin, stainless steel sinks, clothing, instrument delivery surfaces, and other locations can occur. On skin surfaces, the black stain is very difficult to remove, but is harmless and disappears in several days. Some improvement can be accomplished with rubbing the affected area with petroleum jelly, but the black stain is persistent.
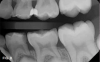
Case 1. A 9-year-old girl had a distal caries lesion of the primary canine tooth and mesial caries of the approximating primary first molar (Figure 1). With no local anesthesia and no discomfort reported by the child, a high-speed diamond bur was used to trim open the contact, exposing the lesions (Figure 2). After the site was air-dried, a flexible interdental pick was used to apply the SDF solution (Figure 3), which was blotted dry with a cotton swab after 60 seconds (Figure 4).
Case 2. This 2-year-old boy had mesial caries lesions of his maxillary central incisors associated with chronic plaque accumulation and lack of tooth brushing or flossing by the parents (Figure 5 and Figure 6). The parents, who were given extensive instructions to remedy the oral hygiene problem, consented to SDF application despite the black discoloration. They related that they not only wanted to avoid a repair appointment for the child, but they also liked the idea that traditional restoration could be delayed until he was older and could more easily tolerate treatment. Three months after initial SDF application, the solution was reapplied (Figure 7).
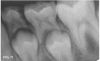
Case 3. This 10-year-old boy was brought to the office for a second opinion regarding restoration of the left primary first molar, which was causing sensitivity (Figure 8). The boy's mother reported that a "tooth-colored filling" had been suggested at another office. The boy was terrified of needle injections and, according to his mother, had required sedation in prior years for restoration of maxillary primary molars. SDF was applied (Figure 9), tooth sensitivity was eliminated, and in 3 months, clinical evaluation and a periapical radiograph confirmed that no other treatment would be needed until the tooth exfoliated (Figure 10 and Figure 11).
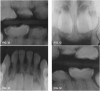
Case 4. At his first dentistry appointment, a 5-year-old with dentinogenesis imperfecta had large caries lesions on the distal of both mandibular primary first molars (Figure 12), along with smaller caries lesions on the distal of the maxillary right primary canine tooth and distal surface of the maxillary right first molar. The distal marginal ridge of the mandibular left second primary molar was fractured and subsequently trimmed smooth, but there was no caries detected in the exposed dentin. Stainless steel crown restoration of the primary first molars would have been difficult to accomplish because of the anatomical form of those teeth, the amount of wear/erosion of the maxillary first molars, and severity of carious destruction of the mandibular first molars. It was predicted that those teeth would be lost to extractions prior to their normal exfoliation time, therefore the goal was to preserve the teeth in place until eruption of the permanent molars to facilitate eventual space maintenance planning. It was thought that SDF could provide an immediate interim solution for caries control for this child, and after this was explained, the boy's father agreed to that treatment immediately at that visit. With cotton roll isolation, top layers of carious tooth substance were debrided from the mandibular first molars using a slow-speed round bur (Figure 13). No anesthetic injections were needed, and the patient related no discomfort. SDF was then painted on the caries lesions of the four teeth (Figure 14), followed by fluoride varnish application (Figure 15). The patient was seen several weeks later for renewed SDF application and dental prophylaxis (Figure 16 and Figure 17).
Case 5. A bite wing radiograph (not shown) revealed a distal caries lesion on a mandibular molar in a 10-year-old girl. The girl's father was informed of the need for treatment to avoid caries spread to the mesial surface of the permanent first molar. He readily agreed to SDF application rather than Class II restoration, so that his daughter could avoid a local anesthetic injection and he could save the expense. With cotton roll isolation and no local anesthetic injection, the distal caries lesion was exposed using a high-speed diamond bur (Figure 18 and Figure 19). Only one application of SDF was used in this case, followed by application of fluoride varnish (Figure 20 and Figure 21). In 7 months, the primary second molar had exfoliated, and only a trace of SDF stain remained on the permanent molar (Figure 22).
Case 6. This 11-year-old had a small fracture of a mesio-occlusal restoration of his primary second molar and marginal caries develop in the long-term Class II restorations in that tooth and the adjacent primary first molar. A bite wing radiograph revealed that those teeth would be exfoliating within 12 to 18 months. SDF was painted around the involved tooth surfaces, and continuing damage from the recurrent caries lesions ceased. Only one SDF coating was used; the teeth were photographed 8 months later (Figure 23).
Case 7. Six months prior, this 12-year old was brought to the office for an emergency visit with a fractured a 6-year-old Class II resin-modified glass-ionomer restoration. Subsequently, he complained that the tooth was sensitive to cold stimulus. After one SDF application, sensitivity was relieved and the tooth remained as shown, until it exfoliated within a year (Figure 24).
Case 8. A 4-year-old newly adopted boy from China was brought to the office for treatment. With nitrous oxide/oxygen inhalation and local anesthesia, a mandibular primary second molar was restored using an MTA pulpotomy and stainless steel crown. His maxillary right primary second molar had a large occlusal caries lesion, along with radiographic and clinical evidence of dento-alveolar abscess. After several days' coverage with antibiotics, the boy returned for extraction of the maxillary molar. With the adoptive mother's consent, after local anesthetic injections were completed and the rubber dam placed, two 60-second applications of silver diammine fluoride were painted into the occlusal caries lesion about 15 minutes before the tooth was extracted (Figure 25). After the extraction, the tooth was sectioned and photographed to observe SDF penetration that had occurred in the 15-minute hiatus (Figure 26).
Silver Diammine Fluoride in Humanitarian Missions
There are a multitude of humanitarian medical and dentistry missions that take dental and medical services to underserved people all over the globe. These programs are planned by religious groups, universities, private dentistry offices, dental societies, and other entities. An example of an ongoing dentistry mission, initiated in 1997 by Doc Bresler's Cavity Busters (www.cavitybusters.com), is the Temple University Haiti Club, which visits Haiti annually with four faculty members and ten dental students to provide treatment to hundreds of people.21 Silver diammine fluoride applications are an excellent adjunct to the restorative and surgical treatments rendered in such missions, especially when no treatment for carious teeth is the alternative due to practical, personnel, and financial restraints.
An example of a medical mission is CI Haiti (www.cihaiti.com), a parish-to-parish group that takes medical services to remote villages in Haiti, providing people with home medical kits and basic medical training and resources. A member of this group, Jesse Leighton, read about silver diammine fluoride in a New York Times article22 and thought SDF treatments could make a valuable addition to their services. Children in the villages have virtually no oral home care and professional dentistry services are hours away and limited. Even if there were local dentists, there is no electricity in the region for routine clinical dentistry equipment. In addition, most children habitually chew on sugar cane, and dental caries is rampant, affecting almost all children and adults. Members of the mission group were given instructions on how to use the silver diammine fluoride solution, and arrangements were made to include SDF applications in their trips. In March 2017, after returning from Haiti and his first experiences with SDF, Mr. Leighton communicated to the authors that "it was quick, easy, and the pain relief for many children was immediate and astonishing." The CI Haiti Mission shows how silver diammine fluoride (Figure 27) can be a valuable adjunct to medical and dental humanitarian missions in parts of the world where no other dental treatment is available.
Conclusion
Silver diammine fluoride treatment has its advantages and disadvantages: the chief disadvantage being black discoloration of treated lesions.19However, with careful case selection, the advantages far outweigh the disadvantages in clinical dentistry for children. In many instances, SDF can offer a useful and practical alternative to traditional primary tooth repair, providing a conservative, workable, and patient-friendly approach that is easily achieved. Regarding treatment success, a recent systematic review and meta-analysis revealed that there is "high quality" evidence that silver diammine fluoride is more effective in controlling dental caries infections than atraumatic restorative treatment, fluoride varnishes, placebo, or no treatment.15 Empirical evidence in many private offices and teaching institutions is bearing that out.
Experiences that dentists are having with SDF in the primary dentition can also be applied to dentistry for permanent teeth. Examples are interception of incipient proximal decalcification and caries lesions16 toothache control "for all ages of bedridden or handicapped people unable to tolerate conventional dental procedures,"19 many indications for caries lesions in geriatric patients, and emergency delaying tactics for people in urgent need of toothache relief and caries abatement while diagnostic services are completed and treatment plans formulated.
About the Author
Theodore P. Croll, DDS
Private Practice
Doylestown, Pennsylvania
Affiliate Professor
Department of Pediatric Dentistry
University of Washington School
of Dentistry
Seattle, Washington
Adjunct Professor
Pediatric Dentistry
University of Texas Health
Science Center
San Antonio, Texas
Joel H. Berg, DDS, MS
Professor
Department of Pediatric Dentistry
University of Washington
School of Dentistry
Seattle, Washington
References
1. Alexander, JW. History of the medical use of silver. Surg Infect (Larchmt). 2009;10(3):289-292.
2. Prinz P. Dental Materia Medica and Therapeutics. 4th ed. St. Louis, MO: C.V. Mosby Company; 1916:217-230.
3.Pedley RD. The Diseases of Children's Teeth: Their Prevention and Treatment. London: JP Segg & Co.; 1895.
4. Hogeboom FE. Filling materials used in deciduous teeth. In: Practical Pedodontia or Juvenile Operative Dentistry and Public Health Dentistry. St. Louis, MO: C.V. Mosby Company; 1924:60-61.
5. Black GV, Black AD: Management of children's teeth. In A work on operative dentistry, Vol. One, The Pathology of the Hard Tissues of the Teeth. 6th ed. Chicago, IL: Medico-Dental Publishing Co; 1924:247-257.
6. Elevate Oral Care. Safety Data Sheet. Advantage Arrest Silver Diamine Fluoride 38%. Rev 01 08/29/16. http://www.elevateoralcare.com/site/images/AASDS082415.pdf. Accessed June 4, 2018.
7. American Academy of Pediatric Dentistry. Chairside guide: Silver diamine fluoride in the management of dental caries lesions. Pediatr Dent. 2017;39(6):478-479.
8. Lou YL, Botelho, MG, Darvell BW. Reaction of silver diamine fluoride [corrected] with hydroxyapatite and protein. Journal of Dentistry. 2011;39(9):612-618.
9. Lou YL, Botelho, MG, Darvell BW. Erratum to "Reaction of silver diammine fluoride with hydroxyapatite and protein" [J. Dent. 39 (2011) 612-618]. Journal of Dentistry. 2012;40(1): 91-93
10. Horst JA, Ellenikiotis H, UCSF Silver Caries Arrest Committee, et al. UCSF protocol for caries arrest using silver diamine fluoride: Rationale, indications and consent. J Calif Dent Assoc. 2016;44(1):16-28.
11. Mei ML, Lo EC, Chu CH. Clinical use of silver diamine fluoride in dental treatment. Compend Contin Educ Dent. 2016;37(2):93-98.
12. Gao S, Zhao I, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: A systematic review. JDR Clin Transl2016;1(3):201-210.
13. Crystal YO, Niederman R. Silver diamine fluoride treatment considerations in children's caries management. Pediatr Dent. 2016; 38(7):466-471.
14. Zhao IS, Gao SS, Hiraishi N, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J. 2018;68(2):67-76.
15. Chibinski AC, Wambier LM, Feltrin J, et al. Silver diamine fluoride has efficacy in controlling caries progression in primary teeth: A systematic review and meta-analysis. Caries Res. 2017;51(5):527-541.
16. Croll TP, Berg J. Delivery of fluoride solutions to proximal tooth surfaces: Part II: Caries interception with silver diamine fluoride. Inside Dentistry. 2017;13(9):56-58.
17. Castillo JL, Rivera S, Aparicio T, et al. The short-term effects of diammine silver fluoride on tooth sensitivity: a randomized controlled trial. J Dent Res. 2011;90(2):203-208.
18. Mei ML, Li QL, Chu CH, et al. Antibacterial effects of silver diamine fluoride on multi-species cariogenic biofilm on caries. Ann Clin Microbiol Antimicrob. 2013;12(2):4.
19. CR Foundation Clinicians Report. 38% Silver diamine fluoride (SDF): Does it arrest dental caries lesion progression? Clinicians Report. 2018;11(1):1-3
20. Croll TP, Nelson TM, MacLean JK. What are the indications and contraindications for use of SDF in anterior teeth? Inside Dentistry. 2018;14(1):30-31
21. The Bresler family is on a mission Pediatric Dentistry Today. 2017;52(6):20-23.
22. Saint Louis C. A cavity-fighting liquid lets kids avoid dentists' drills. New York Times.July 11, 2016.https://www.nytimes.com/2016/07/12/health/silver-diamine-fluoride-dentist-cavities.html. Accessed June 4, 2018.